
Quick Guide to Appeals for Employer-Sponsored & Individual Health Insurance
In Triage Health's free Quick Guide to Appeals for Employer-Sponsored & Individual Health Insurance, you'll learn the difference between internal and external health insurance appeals, appeals before care and after care, and three key steps in the health insurance appeals process.
At some point during your treatment, you may experience a denial of coverage from an insurance company, whether for an imaging scan, prescription drug, treatment, procedure, or genetic test. Most people take “no” for an answer. But those who don’t accept the denial, and file an appeal, may actually win and get coverage for the care prescribed by their health care team up to 60% of the time! Note: if you have a self-funded employer plan the process may be different. Visit our Health Insurance Appeals module at CancerFinances.org for more.
Internal vs. External Appeals
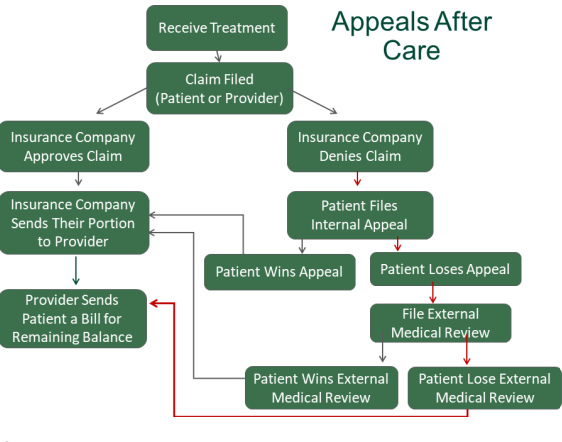
You generally have two chances to appeal a denial of coverage: an internal appeal and an external appeal.
Internal Appeals: When an insurance company has denied coverage for care, you can file an “internal appeal” within your insurance company. Each insurance company has their own internal appeals process, so contact your insurance company for details or look for instructions on how to file an appeal on your denial letter. There are time frames related to filing an internal appeal.
If your insurance company denies your internal appeal, you can request an external appeal. Under the Affordable Care Act, all states must have an external appeals process – this is also sometimes referred to as External Medical Review or Independent Medical Review.
External Appeals: Within four months of receiving your insurance company’s denial of your internal appeal, you can file a written external appeal (note some states provide additional time). External appeals are completed within 45 days of filing and the decision is binding on the insurance company. If urgent, reviews can be expedited, filed at the same time as an internal appeal, and decided within 72 hours. State insurance agencies or the federal Dept. of Health & Human Services administer external appeals. To find the process and contact information for your state, see our free State Resources. The HHS process is free, but states can’t charge more than $25 for an external appeal.
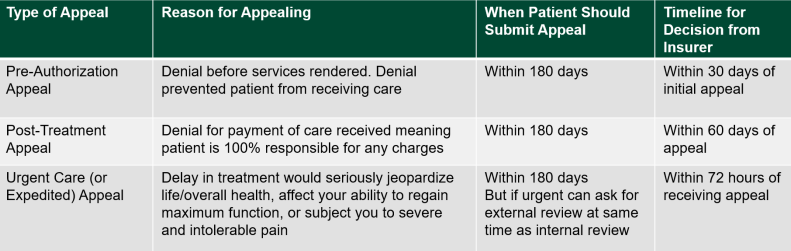
Appeals Before Care vs. After Care
You can file appeals both before and after medical services are provided. The process for filing an appeal before care and after care are slightly different. An example of when you might get a denial of coverage before you even receive care, is when your insurance company requires a pre-authorization before getting care. If your insurance company denies pre-authorization, you can appeal that decision.
For more information:
 Key Steps to the Appeals Process
Key Steps to the Appeals Process
Step 1: Contact Your Insurance Company
- Contact the insurance company to ask for a detailed explanation of your denial and the company’s internal appeals process.
- Keep track of the dates of contact with insurance company representatives, names of individuals you talk to, notes of conversations, and any written documentation you receive. Triage Health has an Health Insurance Appeals Tracking Form.
- Ask family and friends to help you organize bills and insurance documents and take notes during calls with the insurance company.
Step 2: Understand Your Denial
There are several reasons why insurance companies may deny your claim, including:
- Mistakes: Errors can occur relaying patient identifying information, billing details, or CPT/HCPCS codes. Review your bills (don’t be afraid to ask your provider for help), contact your provider and request they resubmit your claim with correct information, and explain the resubmission to your insurance company.
- Pre-Authorization: Insurance companies are not required to pay for care when it has not properly been pre-authorized, so it is very important to note what services require pre-authorization before you get care. If you haven’t gotten a service pre-authorized, ask your insurance company to retroactively authorize it.
- “Experimental or Investigational:” Treatments deemed experimental or investigative by your insurance company may result in denials. Make sure to ask your provider to help when justifying these treatments.
- Service Not Covered: If your insurance company says your service is not covered, check your policy to see if the service is listed as “excluded.” If not, contact your insurance company and ask for more information about the denial. They may claim the service was unnecessary. If so, call your provider and ask for help showing that the care is “medically necessary.”
- Timely Submission: Claims submitted too long after services were provided may be denied. However, if your provider is within network, fixing this error usually only requires a phone call to your provider. As they are in charge of submitting claims, providers are usually held responsible for this mistake.
- Coordination of Benefits (COB): If you have both a primary and a secondary insurance policy, it’s essential to complete and submit COB forms every year. Failing to complete these forms can result in claim denials.
Step 3: Gather Evidence
When gathering evidence for your appeal, make sure to pay attention to the deadlines and requirements for your insurance companies’ internal appeals process. Evidence to support your appeal can include:
- Notes and/or letters of support from your healthcare providers
- Results of tests and procedures related to the care in question
- Relevant medical literature, professional journals, and studies showing the effectiveness of the care, especially when appealing denials of care for being experimental or investigational
- A brief and factual personal statement describing the need for the requested care
Learn More
For more information on navigating finances, visit Navigating Finances & CancerFinances.org.
Sharing Our Quick Guides
We're glad you found this resource helpful! Please feel free to share this resource with your communities or to post a link on your organization's website. If you are a health care professional, we provide free, bulk copies of many of our resources. To make a request, visit TriageHealth.org/MaterialRequest.
However, this content may not be reproduced, in whole or in part, without the express permission of Triage Cancer. Please email us at TriageHealth@TriageCancer.org to request permission.
Last reviewed for updates: 01/2022
Disclaimer: This handout is intended to provide general information on the topics presented. It is provided with the understanding that Triage Cancer is not engaged in rendering any legal, medical, or professional services by its publication or distribution. Although this content was reviewed by a professional, it should not be used as a substitute for professional services. © Triage Cancer 2023
