
Quick Guide to Medicaid Transportation Coverage
This Quick Guide explains what Medicaid non-emergency transportation coverage is, who is eligible, when you can get a ride, how to pay for it, and other rules for using transportation coverage.
Under federal law, every state Medicaid program must provide coverage for non-emergency transportation for people with Medicaid.
Medicaid must cover rides for eligible individuals to and from the doctor’s office, the hospital, or another health care facility for Medicaid-approved care.
But each state’s Medicaid program is different and can have different ways to offer transportation. Also, each state has the option of offering programs that provide more transportation coverage.
Who is Eligible?
To be eligible for transportation coverage, an individual must have Medicaid. States can also require that there be an unmet transportation need, which includes:
- Not having a valid driver’s license;
- Not having a working vehicle available in the household;
- Being unable to travel or wait for services alone; or
- Having a physical, cognitive, mental, or developmental limitation.
To learn about your state’s rules, contact your state Medicaid agency: TriageCancer.org/StateResources.
Steps to When Can You Get a Ride?
Transportation is only covered when it is considered “necessary.” If you have another option for transportation, you might not be eligible. Medicaid transportation also has to: 1) be the least costly and most appropriate option; and 2) provide transport to the nearest qualified provider (with some exceptions).
Here are some examples:
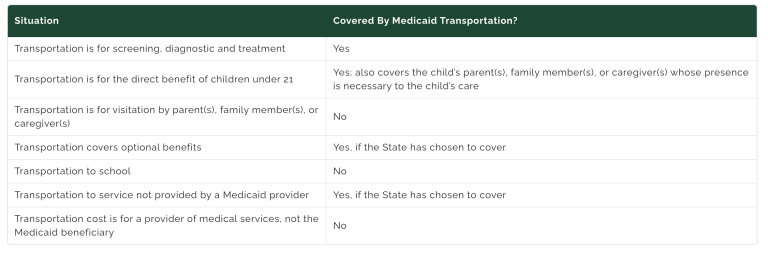
It is important to check your state’s program because it might have more coverage. Some states may cover non-medical transportation, so people can access community services, activities, and resources.
For example, in Texas, non-emergency medical transport services can include rides to the doctor's office, dentist's office, hospital, drug store or any place that provides covered health care services. Money for gas, meals, and lodging related to children 20 and younger, who are staying overnight to get covered health care, and payment for some out-of-state travel for health care may be covered.
Learn More
For more information about Medicaid, visit TriageHealth.org/Medicaid.
Sharing Our Quick Guides
We're glad you found this resource helpful! Please feel free to share this resource with your communities or to post a link on your organization's website. If you are a health care professional, we provide free, bulk copies of many of our resources. To make a request, visit TriageHealth.org/MaterialRequest.
However, this content may not be reproduced, in whole or in part, without the express permission of Triage Cancer. Please email us at TriageHealth@TriageCancer.org to request permission.
Last reviewed for updates: 01/2022
Disclaimer: This handout is intended to provide general information on the topics presented. It is provided with the understanding that Triage Cancer is not engaged in rendering any legal, medical, or professional services by its publication or distribution. Although this content was reviewed by a professional, it should not be used as a substitute for professional services. © Triage Cancer 2023
What Types of Transportation Are Covered?
Transportation may include rides by taxi, car, van, public bus, train, plane, specialized vehicle, or other modes of transport. You might have to share your ride with others.
How Is Transportation Paid For?
Sometimes a Medicaid agency will pay the transportation provider directly. Other times a Medicaid agency might pay you directly.
How Do You Set Up a Ride?
Generally, when you sign up for Medicaid, you will get instructions about when a ride is considered necessary and how to schedule a ride. That may include calling a Medicaid caseworker, a ride service, or another agency for all non-emergency transports. The service should check to:
- Make sure you are eligible for Medicaid;
- Make sure you have an appointment with a Medicaid provider;
- Make sure you have no other reasonable way to get to your appointment; and • Determine what type of ride Medicaid can give you.
States may use different systems to provide transportation. For example, in New York individuals with Medicaid get transportation through a broker. Enrollees who use a private vehicle may be paid back for mileage and expenses that they can document (e.g., receipts).
Tips When Getting Transportation
- Be on time. In some states, Medicaid might not pay for the time a driver waits or might limit how long the driver is allowed to wait for you if you’re not on time.
- Call if you need to cancel a ride. If your appointment changed, call your ride service as soon as you can. If you do not, you could face challenges getting a ride in the future.
- Medicaid will only cover trips to and from a medical facility. If the driver takes you anywhere else, you and the driver could be charged with stealing from Medicaid.
- If a ride does not show up, call the number you used to set up your ride. Also call your medical provider to let them know.
